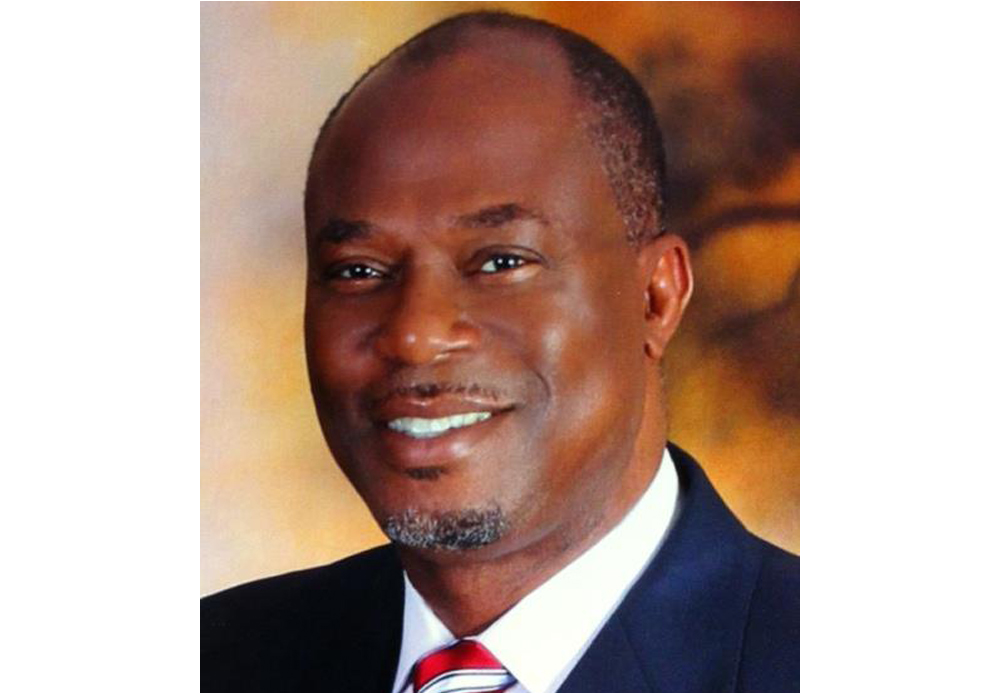
Basil Ubanwa
Northwest Ambulance Services owner charged with 11 count indictment
Contributed By:The 411 News
Submitted fraudulent claims to Medicare, Medicaid for ambulance services
Basil N. Ubanwa, 60 years old, of Crown Point, Indiana, was indicted by a federal grand jury for 11 counts of health care fraud and one count of conspiracy to commit health care fraud, announced U.S. Attorney Thomas Kirsch.
U.S. Attorney Kirsch said, “Health care fraud is a serious crime that drives up the cost of healthcare for all honest Americans. Medicare and Medicaid are not bottomless funds from which theft goes unnoticed or unpunished. Taxpayers are the victims of these crimes. We, with our law enforcement partners, will continue to investigate and aggressively prosecute perpetrators of these fraudulent schemes.”
The indictment alleges that between 2011 and 2018, Ubanwa executed a scheme to obtain hundreds of thousands of dollars by submitting fraudulent claims to Medicare and Medicaid for ambulance services.
From 2007 to 2018, Ubanwa was the owner and manager of Northwest Ambulance Services, located in Crown Point. Northwest’s primary source of revenue was transporting patients to and from kidney dialysis appointments.
According to the indictment, Ubanwa and others directed Northwest employees to transport patients by ambulance who did not qualify for ambulance transportation and who were not eligible to receive such services. Northwest employees were instructed by Ubanwa and others to bill Medicare and Medicaid for services that were not medically necessary and/or were not provided.
The United States is seeking criminal forfeiture of the proceeds of the alleged crimes including, but not limited to, the over $1.9 million from bank accounts associated with Northwest Ambulance and Ubanwa that are listed in the forfeiture count of the indictment.
If convicted in court, any specific sentence to be imposed will be determined by the judge after a consideration of federal sentencing statutes and the Federal Sentencing Guidelines.
This case was investigated by the FBI, Health and Human Services, Office of Inspector General and the Indiana Attorney General’s Medicaid Fraud Control Unit, and is being prosecuted by Assistant United States Attorneys Diane Berkowitz and Abizer Zanzi.
Story Posted:10/18/2018
|